Chicago Indymedia : http://chicago.indymedia.org/archive
News :: Miscellaneous
Circumvention of Medicare law.
The Center for Medicare and Medicaid Services is enabling HMOs to break the law.


Circumvention of the Medicare Grievance and Appeals Process by HMOs and the Center for Medicare and Medicaid Services
Mr. Pich served in the Navy during World War II. Ms. Pich was a registered nurse who interned at the Veteran Administration Hospital in Downey, after World War II. One could say that they served their country well. But with all of the adverse forces in the world today, the Pichs have been hurt the most by an American insurance company, the insurance company?s Chicago area medical providers, and the federal agency that is responsible for enforcing the laws that are supposed to protect the customers of Medicare + Choice (M + C) organizations.
The caseworkers in the offices of the Pich?s federal representatives (Congressman Philip Crane, Senator Peter Fitzgerald, and Senator Richard Durbin) have not been willing to intervene on the Pich?s behalf.
Chapter 13 - Medicare+Choice Beneficiary Grievances, Organization Determinations, and Appeals, of the Medicare Managed Care Manual, is about 80 pages long. It clearly states what is required of M + C organizations, as well as the rights of their enrollees. The Center for Medicare and Medicaid Services (CMS) is enabling Humana Inc. and Advocate Health Care to break these laws.
Whenever a Medicare + Choice Organization (M+C) denies a benefit, they are required by Medicare law to provide written notification to the enrollee. The enrollee then has the right to appeal this organization determination.
The following sections are from Chapter 13 ? M+C Beneficiary Grievances, Organization Determinations, and Appeals in the Medicare Managed Care Manual (May 9, 2003). www.cms.hhs.gov/manuals/116_mmc/mc86toc.asp
10.1 - Definition of Terms
(Rev. 22, 05-09-03)
Unless otherwise stated in this Chapter, the following definitions apply:
Appeal: Any of the procedures that deal with the review of adverse organization determinations on the health care services an enrollee believes he or she is entitled to receive, including delay in providing, arranging for, or approving the health care services (such that a delay would adversely affect the health of the enrollee), or on any amounts the enrollee must pay for a service as defined in 42 CFR 422.566(b). These procedures include reconsideration by the M+C organization and if necessary, an independent review entity, hearings before Administrative Law Judges (ALJs), review by the Departmental Appeals Board (DAB), and judicial review.
40.2.2 - Written Notification by M+C Organizations
(Rev. 22, 05-09-03)
If an enrollee requests an M+C organization to provide a detailed notice of a practitioner's decision to deny a service, in whole or in part, or if the M+C organization decides to deny, in whole or in part, the services or payments then it must give the enrollee a written notice of its determination. If the beneficiary has a representative, the representative must be sent a copy of the notice.
The M+C organization must use approved notice language in Appendix 1. As an alternative, M+C organizations that use electronic EOBs may continue to use the EOB with the standard appeals language on the back in lieu of the standardized Notice of Denial of Payment (NDP). The standardized denial notice forms have been written in a manner that is understandable to the enrollee and provides:
1., The specific reason for the denial that takes into account the enrollee?s presenting medical condition, disabilities, and special language requirements, if any;
2. Information regarding the enrollee's right to a standard or expedited reconsideration and the right to appoint a representative to file an appeal on the enrollee's behalf (as mandated by 42 CFR 422.570 and 422.566(b)(3);
3. For service denials, a description of both the standard and expedited reconsideration processes and timeframes, including conditions for obtaining an expedited reconsideration, and the other elements of the appeals process;
4. For payment denials, a description of the standard reconsideration process and timeframes, and the rest of the appeals process; and
Example of language that is not acceptable in ?40.2.2, list item 1, above (because it is not specific enough or understandable):
You required skilled rehabilitation services-P.T. eval. for mobility + gait-eval. for ADL's, speech eval. swallowing - from 6/5/2001, and these services are no longer needed on a daily basis.
The denial rationale must be specific to each individual case and written in a manner calculated for an enrollee to understand.
Examples of language that is acceptable (because it is specific to the individual's case):
The case file indicated that while Jane Doe was making progress in her therapy programs, her condition had stabilized and further daily skilled services were no longer indicated. The physical therapy notes indicate that she reached her maximum potential in therapy. She had progressed to minimum assistance for bed mobility, moderate assistance with transfers, and was ambulating to 100 feet with a walker. The speech therapist noted that her speech was much improved by 6/12/2001, and that her private caregiver had been instructed on safe swallowing procedures and will continue with feeding responsibilities. The enrollees of a Medicare + Choice have a right to appeal
60.3 - Steps in the Appeals Process
(Rev. 22, 05-09-03)
There are five levels of appeal available to Medicare beneficiaries enrolled in plans offered by M+C Organizations after an adverse organization determination has been made. These levels are to be followed sequentially only if the original denial continues to be upheld at each level by the reviewing entity:
1. Reconsideration of an adverse organization determination by the M+C organization;
2. Reconsideration of an adverse organization determination by the independent review entity;
3. Hearing by an Administrative Law Judge, if at least $100 is at issue;
4. Departmental Appeals Board (DAB) Review; and
5. Judicial Review, if at least $1000 is at issue.
Bette Weisberg is the Director of Managed Care Services at the Center for Medicare and Medicaid Services - Region V, in Chicago. She and her staff are allowing Humana Inc., a Medicare + Choice organization, (M+C), and Advocate Health Centers/Advocate Health Partners (a health care provider) to circumvent the appeals and grievance process. As a result, the enrollees (in this case Constance and Joseph Pich) are not only being denied benefits, they are also being denied their right to appeal.
This is just one example.
My stepfather, Joseph A. Pich, underwent cervical surgery in June 2003 at Lutheran General Hospital in Park Ridge, Illinois. Lutheran General was Mr. Pich?s network hospital at the time of the surgery. Mr. Pich?s neurologist and surgeon, Dr. Rajan Raj (Des Plaines, Illinois), requested that Mr. Pich be evaluated for ?acute? rehabilitation at Lutheran General?s rehabilitation facility (6W) after the surgery.
I know this to be true because Dr. Raj told me. Mr. Pich was evaluated by Dr. Giohn Lee of 6W on June 27, 2003. Dr. Lee?s evaluation did not disqualify Mr. Pich as a candidate for ?acute? rehabilitation. The report states that ??we are going to follow this patient closely and see when he is medically and surgically stable he (sic) is going to need inpatient rehabilitation therapy or not.?
On July 1, 2003, I was told by Dr. Hazienda, a Lutheran General hospitalist (an attending physician other than the Primary Care Physician), that Mr. Pich was not a candidate for ?acute? rehabilitation. This was recorded on page 2 of the Discharge Planning document from Lutheran General. Several of Lutheran General?s social workers then spoke with me about where I wanted Mr. Pich to go for rehabilitation. I was led to believe that Dr. Hazienda?s opinion was the conclusive factor, but it was not. Dr. Lee?s was responsible for making such a decision. Page 2 also states that I was told that Humana would not pay for 6W ?at this time?. I do not recall being told this. The Lutheran General employees, including doctors and social workers, who I spoke with at the time of Mr. Pich?s imminent discharge, emphasized that Mr. Pich was (allegedly) not fit for ?acute? rehabilitation, and from then on there was no further talk about 6W or ?acute? rehabilitation. They did not tell me that Humana had concluded that 6W was ?out of network?. In March 2004, an Advocate caseworker informed me that the only reason that Mr. Pich was not admitted to 6W was because ?insurance denied-out of network?. This was handwritten on Mr. Pich?s 6W inpatient admittance form.
Initially I believed that Mr. Pich was not admitted to 6W solely because he was disqualified as an ?acute? rehabilitation candidate. Had I known the real reason, I would have filed an appeal. Humana never notified us in any form that they were denying a benefit, i.e. that they would not pay for 6W because they had concluded that the rehabilitation services at Lutheran General were ?out of network?. These regulations are stated in section 40.2.2 - Written Notification by M + C Organizations in Chapter 13. The written notification of a denial of a benefit is also supposed to contain the information about an enrollee?s right to appeal. This is how Humana and Advocate denied Mr. Pich his right to appeal their organization determination. In addition, Humana never notified us that the service was not medically necessary, and they did not offer Mr. Pich ?acute? rehabilitation services in a network facility.
I did not want Mr. Pich to be sent to Governors Park (Barrington, Illinois) for rehabilitation, because my mother did not fare well there. Therefore, we were offered Warren-Barr Pavilion (Chicago, Illinois). Warren-Barr is classified as a skilled nursing facility that offers ?sub-acute? rehabilitation services. Mr. Pich was discharged from Lutheran General Hospital, and admitted to Warren-Barr on July 4, 2003. (It should be noted that last year I did not fully realize the difference between ?acute? and ?sub-acute? rehabilitation.)
I was scheduled for heart bypass surgery during this period, so I maintained constant communication with Dr. Judy Heyworth, Mr. Pich?s attending physician at Warren-Barr, and the attending nurse, Nancy Myers. My surgery was postponed several times after July 4, 2003. At one time, it was scheduled for August 20, 2003. On August 18, 2003, I spoke via telephone with Nancy Myers, and she told me that Humana was soon going to stop providing Mr. Pich with rehabilitation. She said that he had reached a plateau. This was not good news, because at the time he was still not yet ambulatory. She told me that he might never walk again. I asked her if she could give me the approximate earliest time that he would need to be discharged from Warren-Barr. She assured me that the earliest date would be August 29, 2003. My surgery was postponed once again, and on August 20, 2003, I received a call from a friend of mine, whose number I had given to Warren-Barr for emergency purposes. He said that somebody from Warren-Barr had called him, and wanted to know where my stepfather would be going when he was discharged on August 22, 2003. I also received somewhat of form letter on or about August 20, notifying us of this decision. (Later, I will discuss more about this letter.)
I immediately phoned Dr. Raj, and told him about Mr. Pich?s poor physical condition, and imminent loss of rehabilitation services. He told me that Mr. Pich should have received the ?acute? rehabilitation, and that the ?sub-acute? was not adequate. I asked Dr. Raj to put this in writing, and he said that he would do so after he returned from a short trip that he was about to take. (Seven months later, he sent an ambiguous statement to me.)
I also called Humana?s Grievance and Appeals Department, and requested an expedited appeal. According to Humana?s Evidence of Coverage booklet, ?if [an enrollee?s] health or ability to function could be seriously harmed by waiting up to 14 calendar days for a standard decision, [the enrollee has a] right to request a decision within 72 hours?. I spoke with one of Humana?s Appeals analysts, and she told me that the matter would be handled as an expedited appeal. However, I agreed to extend the time allowed for an appeal decision, since I wanted Dr. Raj to advise Humana that he disagreed with the decision to give Mr. Pich ?sub-acute? rehabilitation instead of ?acute? rehabilitation.
I received a letter from Humana dated September 8, 2003. Humana had wrongly classified the expedited appeal as a quality of care issue, and referred it to their Quality Management Department for an internal investigation. (Humana claims that the results of such investigations are not subject to disclosure, but that contradicts what is stated in the Medicare Managed Care Manual.)
My numerous requests to Humana for an explanation literally went unanswered. Due to his poor condition, I was forced to place Mr. Pich in another nursing home, this time for custodial care, and this was not covered by insurance. He was transferred from Warren-Barr to Lexington Health Care of Streamwood on August 22, 2003 where he remained until he finally came home on November 22, 2003. One of the reasons why he had to be placed in a nursing home was that I was told that after my surgery, I could not lift anything heavier than 10lbs. Mr. Pich should have been able to walk by August 22, 2003. We maintain that the efficacy of Mr. Pich?s recovery was compromised because he did not receive the ?acute? rehabilitation that Dr. Raj had requested. Fortunately, Mr. Pich is now able to walk, albeit with the aid of a walker.
Humana deliberately misclassified an expedited appeal as a quality issue, in order to avoid having to continue to provide Mr. Pich with rehabilitation services, via an appeal. They avoided another expedited appeal by misleading us as to why he did not receive ?acute ? rehabilitation. We maintain that Mr. Pich was harmed, perhaps irrevocably, by their actions. (In fact, some of the CMS employees in Baltimore and Washington D.C. have responded to me by telling me that it is too late for them to do anything now.)
In 2003, I had limited contact with Jim Coffey of CMS-Region V in Chicago. I had been referred to him by Senator Peter Fitzgerald?s office. Mr. Coffey referred me to the Quality Improvement Organization (QIO). The QIO for Illinois, the Illinois Foundation for Quality Health Care, is located in Iowa. According to Mr. Coffey,
?One of the functions these organizations perform is to investigate complaints that they receive from Medicare beneficiaries who are members of Medicare + Choice plans (or their designated representatives) alleging that the quality of services provided by the plan did not meet professionally recognized standards of health care, including whether appropriate health care services have not been provided or have been provided in inappropriate settings, and whether enrollees have adequate access to health care.?
I spoke with the QIO, but I did not follow through with a complaint at that time, because they do not actually resolve issues.
My next contact with CMS was in January 2004. Mr. Coffey had retired, so I spoke with Maria Gutierrez of Region V in Chicago. I told her about the problems that we were having with Humana and Advocate, and she agreed to investigate. Several weeks after I spoke with her she told me that she did not think that Humana had done anything wrong. I was very unhappy with Ms. Gutierrez.
I next spoke with Mike Kovouras of Region V, and he agreed to investigate my complaints. In March 2004, he informed me that Humana was going to reconsider my appeal about Mr. Pich?s discharge from Warren-Barr. (Since they did not treat it as an appeal in the first place, they were not actually reconsidering it.) Humana subsequently decided that they would pay for the first 28 days that Mr. Pich stayed at Lexington. He received a minimal amount of physical therapy during this period. The therapy that he received at Lexington was even less than what he received at Warren-Barr. He didn?t even have a schedule. Some days he got some, and some days he didn?t. They gave it to him because at the time he arrived at Lexington, he couldn?t walk. It certainly was better than nothing, but it was not anything near what he would have received via an ?acute? facility.
By this time, I had already told Mr. Kavouras that I had just found out that Humana and Advocate had virtually lied to us about why Mr. Pich did not receive ?acute? rehabilitation services. He responded to this news by telling me that he could not do anything about a level of service that I disagreed with. I couldn?t even get him to acknowledge that Dr. Raj had requested the ?acute ?rehabilitation for Mr. Pich. I was very unhappy with Mr. Kavouras.
In fact, CMS in Chicago has been distorting the facts to such a degree that they are now disputing several things that previously had not been a point of contention.
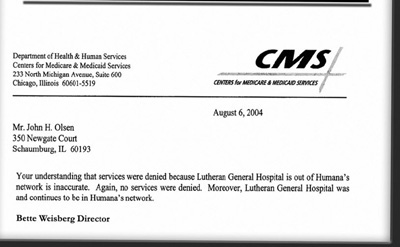
In her August 6, 2004 letter to me, Ms. Weisberg wrote, ?Your understanding that services were denied because Lutheran General Hospital is out of Humana?s network is erroneous.? This statement is false. Nobody ever said that the hospital was out of network. In an April phone call with me, ?Jo? of Humana?s Presidential Inquiry Department acknowledged that Humana denied the benefit because the 6W rehabilitation facility was ?out of network?. I also have several documents from Lutheran General that substantiate this. I am enclosing one that came directly from the rehabilitation unit.
Ms. Weisberg also states that Medicare does not define rehabilitation services as ?acute? or ?sub-acute?. There is a difference between ?acute? rehabilitation and ?sub-acute? rehabilitation. ?Acute? rehabilitation is a program that is much more intense than ?sub-acute?. It is also much more expensive, and that is why more patients are now being referred for ?sub-acute? therapy. Medicare does pay more for ?acute? rehabilitation, regardless of what they call it. For example, ?acute? rehabilitation requires more hours from the therapists, and normally takes place while the patient is in an acute care facility. This too had not previously been a point of contention.
Ms. Weisberg also claims, ??no services were denied? because Mr. Pich received rehabilitation at Warren-Bar Pavilion. This is false. Warren-Barr Pavilion is a skilled nursing care facility that provides ?sub-acute? rehabilitation as opposed to ?acute? rehabilitation.
In fact, based on Ms. Weisberg?s claims, there is no reason that Mr. Pich should have been denied admittance to 6W, but she has so far failed to respond to my request for an explanation.
In this instance alone, Humana and Advocate broke the law several times. They avoided having their organization determinations appealed by us. Not only did Humana fail to notify us in writing, Advocate lied to us about the reason that Mr. Pich had been denied rehabilitation in 6W.
Now I would like to refer back to that August 20, 2003 notice from Advocate. Humana and Advocate have never adhered to section 40.2.2. For example, Advocate?s August 20 letter, notifying Mr. Pich that his ?sub-acute? rehabilitation was soon to be stopped, did not explain in the required manner, why it was being stopped. The notice was basically a form letter, and simply by changing the dates and locations, could be applied to any patient. In fact, the example that the manual gives to illustrate what is not acceptable language contains more information than what Advocate provided in the August 20 letter!
This is from the August 20, 2003 letter to Mr. Pich:
On 8-20-03, we reviewed your medical records and have concluded that you are no longer eligible for skilled nursing care. Therefore, as of August 22,2003, Advocate Health Partners will not pay for any nursing home charges.
You required physical and occupational therapy from 07-04-03 to 08-21-03. Your rehabilitation progress has improved as of 8-21-03 and these services are no longer needed on a daily basis. Therefore, your stay will not be covered by Advocate Health Partners beginning August 22,2003. If you continue your stay beyond this date you will be financially responsible for your stay.
The clinical rationale/criteria used in making the determination is available in writing upon request.
This is what the manual states about unacceptable language:
Example of language that is not acceptable in ?40.2.2, list item 1, above (because it is not specific enough or understandable):
You required skilled rehabilitation services-P.T. eval. for mobility + gait-eval. for ADL's, speech eval. swallowing - from 6/5/2001, and these services are no longer needed on a daily basis.
This is what the manual states about acceptable language:
The denial rationale must be specific to each individual case and written in a manner calculated for an enrollee to understand.
Examples of language that is acceptable (because it is specific to the individual's case):
The case file indicated that while Jane Doe was making progress in her therapy programs, her condition had stabilized and further daily skilled services were no longer indicated. The physical therapy notes indicate that she reached her maximum potential in therapy. She had progressed to minimum assistance for bed mobility, moderate assistance with transfers, and was ambulating to 100 feet with a walker. The speech therapist noted that her speech was much improved by 6/12/2001, and that her private caregiver had been instructed on safe swallowing procedures and will continue with feeding responsibilities. The enrollees of a Medicare + Choice have a right to appeal
I have requested ?the clinical critera/rationale used in making? every determination that Humana and Advocate have ever made about my parents. I have never received a response from either company.
Several weeks ago, Advocate sent me some information defining Medicare coverage in a skilled nursing facility. The pages were copied from a publication titled Complete Guide to Medicare Coverage Issues, published by Ingenix Inc., Salt Lake City, Utah. CMS has told me that this satisfies the requirements stated in 40.2.2.
Advocate did not send us the information that we requested. For example, we were not given the ?denial rationale specific to each individual case? used in deciding that skilled nursing services were no longer needed on a daily basis.
John H. Olsen
Mr. Pich served in the Navy during World War II. Ms. Pich was a registered nurse who interned at the Veteran Administration Hospital in Downey, after World War II. One could say that they served their country well. But with all of the adverse forces in the world today, the Pichs have been hurt the most by an American insurance company, the insurance company?s Chicago area medical providers, and the federal agency that is responsible for enforcing the laws that are supposed to protect the customers of Medicare + Choice (M + C) organizations.
The caseworkers in the offices of the Pich?s federal representatives (Congressman Philip Crane, Senator Peter Fitzgerald, and Senator Richard Durbin) have not been willing to intervene on the Pich?s behalf.
Chapter 13 - Medicare+Choice Beneficiary Grievances, Organization Determinations, and Appeals, of the Medicare Managed Care Manual, is about 80 pages long. It clearly states what is required of M + C organizations, as well as the rights of their enrollees. The Center for Medicare and Medicaid Services (CMS) is enabling Humana Inc. and Advocate Health Care to break these laws.
Whenever a Medicare + Choice Organization (M+C) denies a benefit, they are required by Medicare law to provide written notification to the enrollee. The enrollee then has the right to appeal this organization determination.
The following sections are from Chapter 13 ? M+C Beneficiary Grievances, Organization Determinations, and Appeals in the Medicare Managed Care Manual (May 9, 2003). www.cms.hhs.gov/manuals/116_mmc/mc86toc.asp
10.1 - Definition of Terms
(Rev. 22, 05-09-03)
Unless otherwise stated in this Chapter, the following definitions apply:
Appeal: Any of the procedures that deal with the review of adverse organization determinations on the health care services an enrollee believes he or she is entitled to receive, including delay in providing, arranging for, or approving the health care services (such that a delay would adversely affect the health of the enrollee), or on any amounts the enrollee must pay for a service as defined in 42 CFR 422.566(b). These procedures include reconsideration by the M+C organization and if necessary, an independent review entity, hearings before Administrative Law Judges (ALJs), review by the Departmental Appeals Board (DAB), and judicial review.
40.2.2 - Written Notification by M+C Organizations
(Rev. 22, 05-09-03)
If an enrollee requests an M+C organization to provide a detailed notice of a practitioner's decision to deny a service, in whole or in part, or if the M+C organization decides to deny, in whole or in part, the services or payments then it must give the enrollee a written notice of its determination. If the beneficiary has a representative, the representative must be sent a copy of the notice.
The M+C organization must use approved notice language in Appendix 1. As an alternative, M+C organizations that use electronic EOBs may continue to use the EOB with the standard appeals language on the back in lieu of the standardized Notice of Denial of Payment (NDP). The standardized denial notice forms have been written in a manner that is understandable to the enrollee and provides:
1., The specific reason for the denial that takes into account the enrollee?s presenting medical condition, disabilities, and special language requirements, if any;
2. Information regarding the enrollee's right to a standard or expedited reconsideration and the right to appoint a representative to file an appeal on the enrollee's behalf (as mandated by 42 CFR 422.570 and 422.566(b)(3);
3. For service denials, a description of both the standard and expedited reconsideration processes and timeframes, including conditions for obtaining an expedited reconsideration, and the other elements of the appeals process;
4. For payment denials, a description of the standard reconsideration process and timeframes, and the rest of the appeals process; and
Example of language that is not acceptable in ?40.2.2, list item 1, above (because it is not specific enough or understandable):
You required skilled rehabilitation services-P.T. eval. for mobility + gait-eval. for ADL's, speech eval. swallowing - from 6/5/2001, and these services are no longer needed on a daily basis.
The denial rationale must be specific to each individual case and written in a manner calculated for an enrollee to understand.
Examples of language that is acceptable (because it is specific to the individual's case):
The case file indicated that while Jane Doe was making progress in her therapy programs, her condition had stabilized and further daily skilled services were no longer indicated. The physical therapy notes indicate that she reached her maximum potential in therapy. She had progressed to minimum assistance for bed mobility, moderate assistance with transfers, and was ambulating to 100 feet with a walker. The speech therapist noted that her speech was much improved by 6/12/2001, and that her private caregiver had been instructed on safe swallowing procedures and will continue with feeding responsibilities. The enrollees of a Medicare + Choice have a right to appeal
60.3 - Steps in the Appeals Process
(Rev. 22, 05-09-03)
There are five levels of appeal available to Medicare beneficiaries enrolled in plans offered by M+C Organizations after an adverse organization determination has been made. These levels are to be followed sequentially only if the original denial continues to be upheld at each level by the reviewing entity:
1. Reconsideration of an adverse organization determination by the M+C organization;
2. Reconsideration of an adverse organization determination by the independent review entity;
3. Hearing by an Administrative Law Judge, if at least $100 is at issue;
4. Departmental Appeals Board (DAB) Review; and
5. Judicial Review, if at least $1000 is at issue.
Bette Weisberg is the Director of Managed Care Services at the Center for Medicare and Medicaid Services - Region V, in Chicago. She and her staff are allowing Humana Inc., a Medicare + Choice organization, (M+C), and Advocate Health Centers/Advocate Health Partners (a health care provider) to circumvent the appeals and grievance process. As a result, the enrollees (in this case Constance and Joseph Pich) are not only being denied benefits, they are also being denied their right to appeal.
This is just one example.
My stepfather, Joseph A. Pich, underwent cervical surgery in June 2003 at Lutheran General Hospital in Park Ridge, Illinois. Lutheran General was Mr. Pich?s network hospital at the time of the surgery. Mr. Pich?s neurologist and surgeon, Dr. Rajan Raj (Des Plaines, Illinois), requested that Mr. Pich be evaluated for ?acute? rehabilitation at Lutheran General?s rehabilitation facility (6W) after the surgery.
I know this to be true because Dr. Raj told me. Mr. Pich was evaluated by Dr. Giohn Lee of 6W on June 27, 2003. Dr. Lee?s evaluation did not disqualify Mr. Pich as a candidate for ?acute? rehabilitation. The report states that ??we are going to follow this patient closely and see when he is medically and surgically stable he (sic) is going to need inpatient rehabilitation therapy or not.?
On July 1, 2003, I was told by Dr. Hazienda, a Lutheran General hospitalist (an attending physician other than the Primary Care Physician), that Mr. Pich was not a candidate for ?acute? rehabilitation. This was recorded on page 2 of the Discharge Planning document from Lutheran General. Several of Lutheran General?s social workers then spoke with me about where I wanted Mr. Pich to go for rehabilitation. I was led to believe that Dr. Hazienda?s opinion was the conclusive factor, but it was not. Dr. Lee?s was responsible for making such a decision. Page 2 also states that I was told that Humana would not pay for 6W ?at this time?. I do not recall being told this. The Lutheran General employees, including doctors and social workers, who I spoke with at the time of Mr. Pich?s imminent discharge, emphasized that Mr. Pich was (allegedly) not fit for ?acute? rehabilitation, and from then on there was no further talk about 6W or ?acute? rehabilitation. They did not tell me that Humana had concluded that 6W was ?out of network?. In March 2004, an Advocate caseworker informed me that the only reason that Mr. Pich was not admitted to 6W was because ?insurance denied-out of network?. This was handwritten on Mr. Pich?s 6W inpatient admittance form.
Initially I believed that Mr. Pich was not admitted to 6W solely because he was disqualified as an ?acute? rehabilitation candidate. Had I known the real reason, I would have filed an appeal. Humana never notified us in any form that they were denying a benefit, i.e. that they would not pay for 6W because they had concluded that the rehabilitation services at Lutheran General were ?out of network?. These regulations are stated in section 40.2.2 - Written Notification by M + C Organizations in Chapter 13. The written notification of a denial of a benefit is also supposed to contain the information about an enrollee?s right to appeal. This is how Humana and Advocate denied Mr. Pich his right to appeal their organization determination. In addition, Humana never notified us that the service was not medically necessary, and they did not offer Mr. Pich ?acute? rehabilitation services in a network facility.
I did not want Mr. Pich to be sent to Governors Park (Barrington, Illinois) for rehabilitation, because my mother did not fare well there. Therefore, we were offered Warren-Barr Pavilion (Chicago, Illinois). Warren-Barr is classified as a skilled nursing facility that offers ?sub-acute? rehabilitation services. Mr. Pich was discharged from Lutheran General Hospital, and admitted to Warren-Barr on July 4, 2003. (It should be noted that last year I did not fully realize the difference between ?acute? and ?sub-acute? rehabilitation.)
I was scheduled for heart bypass surgery during this period, so I maintained constant communication with Dr. Judy Heyworth, Mr. Pich?s attending physician at Warren-Barr, and the attending nurse, Nancy Myers. My surgery was postponed several times after July 4, 2003. At one time, it was scheduled for August 20, 2003. On August 18, 2003, I spoke via telephone with Nancy Myers, and she told me that Humana was soon going to stop providing Mr. Pich with rehabilitation. She said that he had reached a plateau. This was not good news, because at the time he was still not yet ambulatory. She told me that he might never walk again. I asked her if she could give me the approximate earliest time that he would need to be discharged from Warren-Barr. She assured me that the earliest date would be August 29, 2003. My surgery was postponed once again, and on August 20, 2003, I received a call from a friend of mine, whose number I had given to Warren-Barr for emergency purposes. He said that somebody from Warren-Barr had called him, and wanted to know where my stepfather would be going when he was discharged on August 22, 2003. I also received somewhat of form letter on or about August 20, notifying us of this decision. (Later, I will discuss more about this letter.)
I immediately phoned Dr. Raj, and told him about Mr. Pich?s poor physical condition, and imminent loss of rehabilitation services. He told me that Mr. Pich should have received the ?acute? rehabilitation, and that the ?sub-acute? was not adequate. I asked Dr. Raj to put this in writing, and he said that he would do so after he returned from a short trip that he was about to take. (Seven months later, he sent an ambiguous statement to me.)
I also called Humana?s Grievance and Appeals Department, and requested an expedited appeal. According to Humana?s Evidence of Coverage booklet, ?if [an enrollee?s] health or ability to function could be seriously harmed by waiting up to 14 calendar days for a standard decision, [the enrollee has a] right to request a decision within 72 hours?. I spoke with one of Humana?s Appeals analysts, and she told me that the matter would be handled as an expedited appeal. However, I agreed to extend the time allowed for an appeal decision, since I wanted Dr. Raj to advise Humana that he disagreed with the decision to give Mr. Pich ?sub-acute? rehabilitation instead of ?acute? rehabilitation.
I received a letter from Humana dated September 8, 2003. Humana had wrongly classified the expedited appeal as a quality of care issue, and referred it to their Quality Management Department for an internal investigation. (Humana claims that the results of such investigations are not subject to disclosure, but that contradicts what is stated in the Medicare Managed Care Manual.)
My numerous requests to Humana for an explanation literally went unanswered. Due to his poor condition, I was forced to place Mr. Pich in another nursing home, this time for custodial care, and this was not covered by insurance. He was transferred from Warren-Barr to Lexington Health Care of Streamwood on August 22, 2003 where he remained until he finally came home on November 22, 2003. One of the reasons why he had to be placed in a nursing home was that I was told that after my surgery, I could not lift anything heavier than 10lbs. Mr. Pich should have been able to walk by August 22, 2003. We maintain that the efficacy of Mr. Pich?s recovery was compromised because he did not receive the ?acute? rehabilitation that Dr. Raj had requested. Fortunately, Mr. Pich is now able to walk, albeit with the aid of a walker.
Humana deliberately misclassified an expedited appeal as a quality issue, in order to avoid having to continue to provide Mr. Pich with rehabilitation services, via an appeal. They avoided another expedited appeal by misleading us as to why he did not receive ?acute ? rehabilitation. We maintain that Mr. Pich was harmed, perhaps irrevocably, by their actions. (In fact, some of the CMS employees in Baltimore and Washington D.C. have responded to me by telling me that it is too late for them to do anything now.)
In 2003, I had limited contact with Jim Coffey of CMS-Region V in Chicago. I had been referred to him by Senator Peter Fitzgerald?s office. Mr. Coffey referred me to the Quality Improvement Organization (QIO). The QIO for Illinois, the Illinois Foundation for Quality Health Care, is located in Iowa. According to Mr. Coffey,
?One of the functions these organizations perform is to investigate complaints that they receive from Medicare beneficiaries who are members of Medicare + Choice plans (or their designated representatives) alleging that the quality of services provided by the plan did not meet professionally recognized standards of health care, including whether appropriate health care services have not been provided or have been provided in inappropriate settings, and whether enrollees have adequate access to health care.?
I spoke with the QIO, but I did not follow through with a complaint at that time, because they do not actually resolve issues.
My next contact with CMS was in January 2004. Mr. Coffey had retired, so I spoke with Maria Gutierrez of Region V in Chicago. I told her about the problems that we were having with Humana and Advocate, and she agreed to investigate. Several weeks after I spoke with her she told me that she did not think that Humana had done anything wrong. I was very unhappy with Ms. Gutierrez.
I next spoke with Mike Kovouras of Region V, and he agreed to investigate my complaints. In March 2004, he informed me that Humana was going to reconsider my appeal about Mr. Pich?s discharge from Warren-Barr. (Since they did not treat it as an appeal in the first place, they were not actually reconsidering it.) Humana subsequently decided that they would pay for the first 28 days that Mr. Pich stayed at Lexington. He received a minimal amount of physical therapy during this period. The therapy that he received at Lexington was even less than what he received at Warren-Barr. He didn?t even have a schedule. Some days he got some, and some days he didn?t. They gave it to him because at the time he arrived at Lexington, he couldn?t walk. It certainly was better than nothing, but it was not anything near what he would have received via an ?acute? facility.
By this time, I had already told Mr. Kavouras that I had just found out that Humana and Advocate had virtually lied to us about why Mr. Pich did not receive ?acute? rehabilitation services. He responded to this news by telling me that he could not do anything about a level of service that I disagreed with. I couldn?t even get him to acknowledge that Dr. Raj had requested the ?acute ?rehabilitation for Mr. Pich. I was very unhappy with Mr. Kavouras.
In fact, CMS in Chicago has been distorting the facts to such a degree that they are now disputing several things that previously had not been a point of contention.
In her August 6, 2004 letter to me, Ms. Weisberg wrote, ?Your understanding that services were denied because Lutheran General Hospital is out of Humana?s network is erroneous.? This statement is false. Nobody ever said that the hospital was out of network. In an April phone call with me, ?Jo? of Humana?s Presidential Inquiry Department acknowledged that Humana denied the benefit because the 6W rehabilitation facility was ?out of network?. I also have several documents from Lutheran General that substantiate this. I am enclosing one that came directly from the rehabilitation unit.
Ms. Weisberg also states that Medicare does not define rehabilitation services as ?acute? or ?sub-acute?. There is a difference between ?acute? rehabilitation and ?sub-acute? rehabilitation. ?Acute? rehabilitation is a program that is much more intense than ?sub-acute?. It is also much more expensive, and that is why more patients are now being referred for ?sub-acute? therapy. Medicare does pay more for ?acute? rehabilitation, regardless of what they call it. For example, ?acute? rehabilitation requires more hours from the therapists, and normally takes place while the patient is in an acute care facility. This too had not previously been a point of contention.
Ms. Weisberg also claims, ??no services were denied? because Mr. Pich received rehabilitation at Warren-Bar Pavilion. This is false. Warren-Barr Pavilion is a skilled nursing care facility that provides ?sub-acute? rehabilitation as opposed to ?acute? rehabilitation.
In fact, based on Ms. Weisberg?s claims, there is no reason that Mr. Pich should have been denied admittance to 6W, but she has so far failed to respond to my request for an explanation.
In this instance alone, Humana and Advocate broke the law several times. They avoided having their organization determinations appealed by us. Not only did Humana fail to notify us in writing, Advocate lied to us about the reason that Mr. Pich had been denied rehabilitation in 6W.
Now I would like to refer back to that August 20, 2003 notice from Advocate. Humana and Advocate have never adhered to section 40.2.2. For example, Advocate?s August 20 letter, notifying Mr. Pich that his ?sub-acute? rehabilitation was soon to be stopped, did not explain in the required manner, why it was being stopped. The notice was basically a form letter, and simply by changing the dates and locations, could be applied to any patient. In fact, the example that the manual gives to illustrate what is not acceptable language contains more information than what Advocate provided in the August 20 letter!
This is from the August 20, 2003 letter to Mr. Pich:
On 8-20-03, we reviewed your medical records and have concluded that you are no longer eligible for skilled nursing care. Therefore, as of August 22,2003, Advocate Health Partners will not pay for any nursing home charges.
You required physical and occupational therapy from 07-04-03 to 08-21-03. Your rehabilitation progress has improved as of 8-21-03 and these services are no longer needed on a daily basis. Therefore, your stay will not be covered by Advocate Health Partners beginning August 22,2003. If you continue your stay beyond this date you will be financially responsible for your stay.
The clinical rationale/criteria used in making the determination is available in writing upon request.
This is what the manual states about unacceptable language:
Example of language that is not acceptable in ?40.2.2, list item 1, above (because it is not specific enough or understandable):
You required skilled rehabilitation services-P.T. eval. for mobility + gait-eval. for ADL's, speech eval. swallowing - from 6/5/2001, and these services are no longer needed on a daily basis.
This is what the manual states about acceptable language:
The denial rationale must be specific to each individual case and written in a manner calculated for an enrollee to understand.
Examples of language that is acceptable (because it is specific to the individual's case):
The case file indicated that while Jane Doe was making progress in her therapy programs, her condition had stabilized and further daily skilled services were no longer indicated. The physical therapy notes indicate that she reached her maximum potential in therapy. She had progressed to minimum assistance for bed mobility, moderate assistance with transfers, and was ambulating to 100 feet with a walker. The speech therapist noted that her speech was much improved by 6/12/2001, and that her private caregiver had been instructed on safe swallowing procedures and will continue with feeding responsibilities. The enrollees of a Medicare + Choice have a right to appeal
I have requested ?the clinical critera/rationale used in making? every determination that Humana and Advocate have ever made about my parents. I have never received a response from either company.
Several weeks ago, Advocate sent me some information defining Medicare coverage in a skilled nursing facility. The pages were copied from a publication titled Complete Guide to Medicare Coverage Issues, published by Ingenix Inc., Salt Lake City, Utah. CMS has told me that this satisfies the requirements stated in 40.2.2.
Advocate did not send us the information that we requested. For example, we were not given the ?denial rationale specific to each individual case? used in deciding that skilled nursing services were no longer needed on a daily basis.
John H. Olsen
Information Library
Views
Search
Account Login
Media Centers
- worcester
- western mass
- vermont
- urbana-champaign
- tennessee
- tampa bay
- seattle
- sarasota
- santa cruz, ca
- santa barbara
- san francisco bay area
- san francisco
- san diego
- saint louis
- rogue valley
- rochester
- richmond
- portland
- pittsburgh
- philadelphia
- oklahoma
- nyc
- north texas
- north carolina
- new orleans
- new mexico
- new hampshire
- minneapolis/st. paul
- milwaukee
- michigan
- miami
- maine
- madison
- la
- kansas city
- hudson mohawk
- houston
- hawaii
- dc
- columbus
- colorado
- cleveland
- chicago
- charlottesville
- buffalo
- boston
- binghamton
- big muddy
- baltimore
- austin indymedia
- austin
- atlanta
- asheville
- arkansas
- arizona
- valencia
- united kingdom
- ukraine
- toulouse
- toscana
- torun
- switzerland
- sverige
- scotland
- sardegna
- russia
- romania
- roma
- portugal
- poland
- piemonte
- patras
- paris/Île-de-france
- oost-vlaanderen
- nottingham
- norway
- northern england
- nice
- netherlands
- napoli
- nantes
- marseille
- malta
- madrid
- london
- lombardia
- linksunten
- lille
- liguria
- liege
- la plana
- italy
- istanbul
- ireland
- hungary
- grenoble
- germany
- galiza
- euskal herria
- estrecho / madiaq
- emilia-romagna
- cyprus
- croatia
- calabria
- bulgaria
- brussels
- bristol
- belgrade
- belgium
- belarus
- barcelona
- austria
- athens
- armenia
- antwerpen
- andorra
- alacant
- abruzzo
This site made manifest by dadaIMC software



